Does Medicare Pay for Compression Stockings? A Quick Guide
Summary
So, does Medicare pay for compression stockings? The short answer is yes—under specific circumstances. Medicare typically covers compression stockings if they are deemed medically necessary, particularly for individuals with conditions like chronic venous insufficiency (CVI) or other vein diseases.
If you’re considering compression stockings, you may be wondering: does Medicare pay for compression stockings? The answer isn’t a simple yes or no. While Medicare may provide coverage, certain conditions must be met to qualify for reimbursement. Compression stockings can be essential to managing venous conditions like varicose veins and chronic venous insufficiency (CVI), so understanding your coverage is important.
At Vein Treatment Clinic, we aim to help you navigate the complexities of insurance coverage. With locations in New York, Long Island, California, Maryland, and New Jersey, our team of vein specialists can guide you through determining if your Medicare plan will cover compression stockings and how to maximize your benefits. Let’s dive into the details!
Are you interested in getting more information about your condition or getting a treatment?
Fill the form below to start!
Does Medicare Pay for Compression Stockings?
Medicare Part B can cover compression stockings if your vein doctor deems them medically necessary. Generally, compression stockings are prescribed to help manage symptoms associated with vein conditions, such as chronic venous insufficiency or varicose veins. If these conditions are diagnosed, compression stockings can help improve blood flow and prevent worsening symptoms, such as swelling and discomfort.
However, Medicare doesn’t provide blanket coverage for all types of compression stockings. The coverage depends on the conditions prescribed and whether your healthcare provider documents their necessity for managing a medical condition. If compression stockings are deemed part of your vein treatment, Medicare may approve coverage.
Factors That Determine If Medicare Will Pay for Compression Stockings
Medicare does not automatically cover compression stockings, so it’s important to understand the various factors that will influence approval. These include your diagnosis, medical history, and the type of compression stockings prescribed. Below are the key factors that determine if you qualify for Medicare coverage.
Diagnosis of Chronic Venous Insufficiency (CVI)
One of the factors influencing whether Medicare covers compression stockings is if you have been diagnosed with chronic venous insufficiency (CVI). CVI is a condition in which the veins in your legs cannot efficiently return blood to your heart, leading to swelling and varicose veins.
If your healthcare provider diagnoses you with CVI, compression stockings can play a critical role in alleviating symptoms and preventing further complications. As such, Medicare is more likely to approve coverage for compression stockings when they are prescribed as part of a treatment plan for CVI.
Medical Necessity
Medicare only covers compression stockings when they are considered medically necessary to treat an underlying condition, such as varicose veins, deep vein thrombosis (DVT), or CVI. Simply using compression stockings for cosmetic reasons, such as improving appearance or preventing mild discomfort, may not meet the criteria for coverage.
Your vein doctor will need to provide appropriate documentation showing that the stockings are needed to manage a medical condition and that they are part of an overall treatment plan.
Type of Compression Stockings
Not all compression stockings are the same, and Medicare will typically only cover specific types. The stockings must meet certain standards, including a minimum compression level (usually 20-30 mmHg). Your vein doctor will prescribe the appropriate type based on your needs, and Medicare will only cover the cost if they meet the necessary specifications.
Your Vein Doctor’s Documentation
To receive Medicare coverage for compression stockings, your vein doctor must document that they are medically necessary. This may include details of your diagnosis, the severity of your symptoms, and how compression stockings are part of your vein treatment plan.
Without this, Medicare is unlikely to approve coverage. Ensure your vein doctor understands the importance of thorough documentation to improve your chances of getting your compression stockings covered.
How Vein Treatment Clinic Helps You Maximize Insurance Coverage
At Vein Treatment Clinic, we understand that navigating insurance and Medicare can be overwhelming. Our team is dedicated to ensuring you maximize your benefits and receive the coverage you’re entitled to. Here’s how we can help:
Insurance Verification Assistance
Before your first appointment, we work with you to verify your insurance details. This ensures you understand what is covered under your plan, including whether compression stockings are eligible for reimbursement. By doing this ahead of time, we can avoid any surprises and ensure you get the most out of your benefits.
Comprehensive Documentation Support
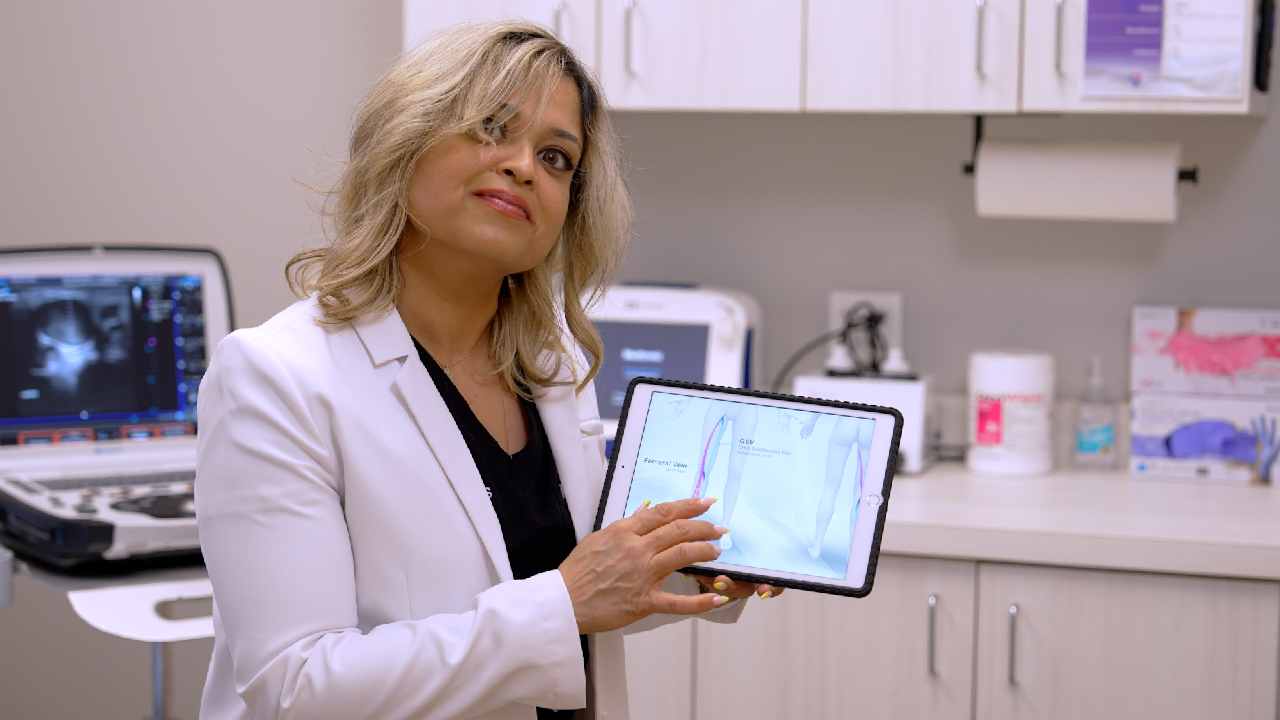
We submit the necessary records, including your diagnosis and the medical necessity of the treatment. At Vein Treatment Clinic, we use duplex ultrasound to provide clear, visual proof of conditions like chronic venous insufficiency. This documentation significantly improves the chances of your compression stockings being covered.
Guidance Through the Process
The process of obtaining Medicare coverage for compression stockings can be complicated. Our experts will walk you through every step, from the initial consultation to the approval of your vein treatment. If there are any issues, we will strongly advocate for you.
FAQs
Do varicose veins go away?
Do varicose veins go away? Unfortunately, varicose veins do not go away on their own. Treatment options, such as endovenous laser ablation or sclerotherapy, can help manage symptoms and improve the appearance of varicose veins. If you’re dealing with varicose veins, it’s essential to consult a vein specialist to explore your vein treatment options.
Can varicose veins go away?
Can varicose veins go away? While varicose veins may not go away by themselves, they can be effectively treated. Minimally invasive vein treatments like radiofrequency ablation or VenaSeal are highly effective in treating the root cause of varicose veins, leading to long-term relief and improved leg health.
Where can I find spider vein removal near me?
If you’re searching for spider vein removal near me, Vein Treatment Clinic has locations across New York, Long Island, California, Maryland, and New Jersey. We specialize in treatments like sclerotherapy and laser ablation to remove spider veins.
How to get rid of veins on legs?
If you’re wondering how to get rid of veins on legs, treatments like endovenous laser ablation and VenaSeal can provide long-lasting results by targeting the underlying vein issue. These vein treatments are minimally invasive and highly effective.
How to get insurance to pay for varicose vein removal?
To get insurance to pay for varicose vein removal, it’s important to have documentation showing that the treatment is medically necessary, not just cosmetic. Vein Treatment Clinic works with most insurance providers to ensure that medically necessary treatments, including varicose vein removal, are covered. Contact us to verify your insurance details today.
Medicare can pay for compression stockings when they are prescribed for a medically necessary condition like chronic venous insufficiency. By understanding the factors involved and working with experts, you can ensure your vein treatment is covered.
At Vein Treatment Clinic, we are here to assist with insurance verification and provide the support you need to get the care you deserve. Contact us to schedule a consultation and learn how we can help you maximize your insurance benefits.
FEATURED POSTS BY VEIN DOCTORS