Do All Insurance Companies Cover Varicose Vein Treatments?
You’ve been struggling with swollen, aching legs for months. Standing for extended periods leaves your legs heavy and tired, and visible varicose veins or spider veins have made you self-conscious about wearing shorts or skirts. You’ve finally decided to seek professional help, but one pressing question lingers—will your medical insurance cover the treatment?
At Vein Treatment Clinic, we understand the uncertainty surrounding insurance coverage for varicose veins treatments. Navigating the medical insurance system in the USA can be difficult, especially when American healthcare costs vary widely. That’s why we’re here to guide you every step of the way. With state-of-the-art vein treatment clinics across New York, New Jersey, Long Island, California, and Maryland, we accept most medical insurances and help verify your insurance details to make your treatment as stress-free as possible.
Are you interested in getting more information about your condition or getting a treatment?
Fill the form below to start!
Insurance Coverage for Varicose Vein Treatments
Medical insurance usually covers varicose vein treatments if deemed medically necessary. Treatments are typically considered medically necessary if your varicose veins are causing symptoms such as leg pain, swelling, cramping, or skin changes. These symptoms are often linked to an underlying condition known as venous insufficiency, which affects the proper flow of blood in your veins. Once a diagnosis of venous insufficiency is confirmed through a duplex ultrasound, insurance companies in the USA are more likely to approve treatment.
It’s worth noting that spider veins, smaller and less prominent than varicose veins, are often categorized as cosmetic concerns. However, if your spider veins are caused by venous insufficiency, spider vein treatments may also qualify for insurance coverage. In such cases, your vein doctor may include sclerotherapy and ambulatory phlebectomy, which focuses on removing visible spider veins and small varicose veins, into your overall vein treatment plan.
Why Doesn’t Every Insurance Company Cover Varicose Vein Treatments?
Insurance coverage can vary significantly between providers and plans. The medical insurance system in the USA includes different types of policies, each with its terms, deductibles, and exclusions. While most insurance companies in the USA provide coverage for medically necessary vein treatments, the specific criteria and approval processes can differ. This variability means some insurance providers may require additional documentation or evidence of your symptoms before approving varicose vein treatments.
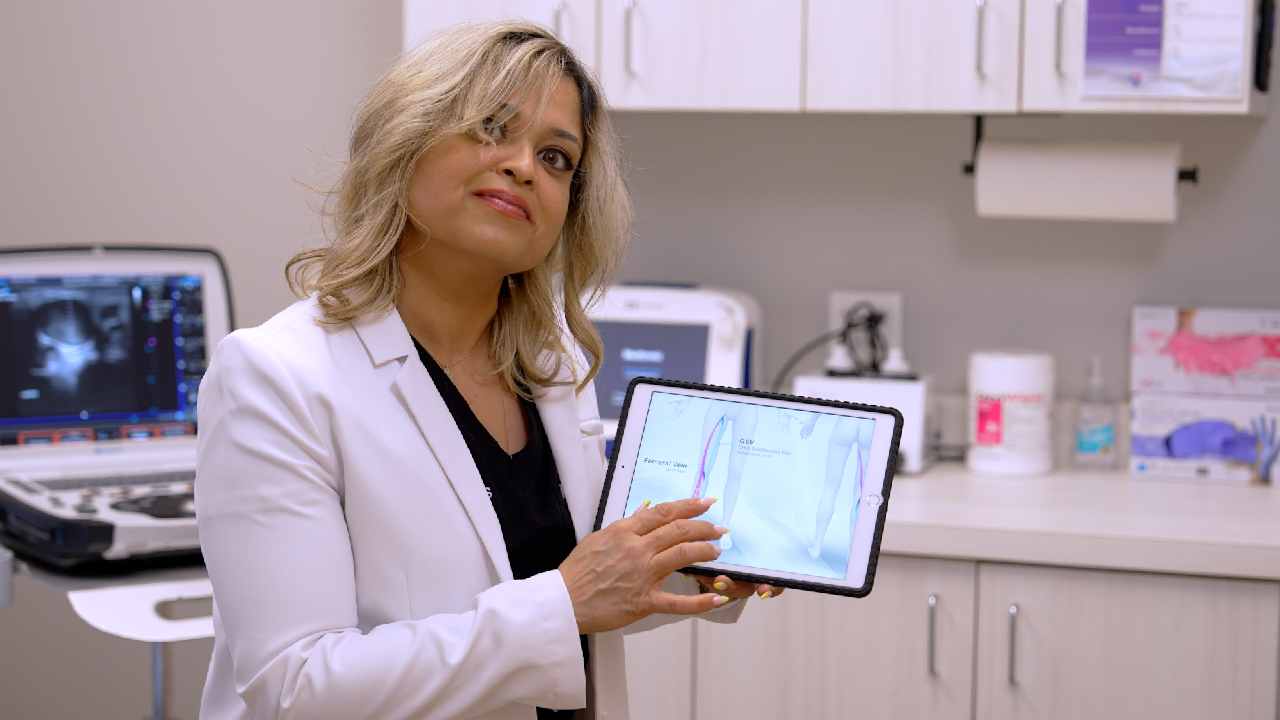
Another factor influencing coverage is the perception of varicose vein treatments as cosmetic. Many insurance companies evaluate whether the procedure addresses a medical issue or enhances appearance. Procedures deemed cosmetic are typically not covered, so a thorough medical evaluation is crucial. At Vein Treatment Clinic, our board-certified vein doctors use duplex ultrasound to diagnose underlying venous insufficiency and provide documentation that proves the necessity of varicose vein treatments, thus helping with insurance.
How Much Does Insurance Cover for Varicose Vein Treatments?
The extent of insurance coverage depends on your specific plan and the recommended treatment. Common minimally invasive vein treatments, such as sclerotherapy, endovenous laser ablation, and radiofrequency ablation, are generally covered by medical insurance if necessary. However, out-of-pocket costs can still vary based on your deductible, co-pay, and coverage limits.
Vein Treatment Clinic offers insurance verification before your first appointment to ease this process. Our insurance specialists tirelessly maximize your coverage and minimize your financial burden. If you’re wondering how much insurance might cover for your treatment, contact us to schedule a consultation and request insurance verification.
The Importance of Choosing the Right Vein Treatment Clinic
The medical insurance system in the USA is complex, but the right vein clinic can make all the difference. Vein Treatment Clinic has extensive partnerships with all insurance companies, enabling us to advocate effectively for your coverage. Our team submits all necessary documentation, such as ultrasound results and physician recommendations, to support your claim. We take pride in handling the insurance process so you can focus on your health.
Our vein treatment clinics, located in convenient areas across the country, are equipped with advanced diagnostic tools to identify the root cause of your varicose veins. By providing a comprehensive evaluation, we help ensure your treatment plan meets the medical necessity criteria required by most insurance providers.
Why Addressing Varicose Veins Early Matters
If left untreated, varicose veins and venous insufficiency can lead to complications such as skin ulcers, blood clots, or deep vein thrombosis. Addressing these issues early improves quality of life and can prevent more invasive and costly treatments in the future. Most of our vein treatments are minimally invasive, performed in outpatient settings, and require little to no downtime, making them an efficient option for managing venous conditions.
What to Expect at Vein Treatment Clinic
At Vein Treatment Clinic, we begin with a detailed consultation to assess your symptoms and concerns. Our registered physicians in vascular interpretation use duplex ultrasound to diagnose venous insufficiency or other underlying issues. This step is crucial for determining whether your vein treatment may qualify as medically necessary.
Once your diagnosis is confirmed, our vein specialists curate a treatment plan tailored to your needs. We offer a range of minimally invasive procedures, including sclerotherapy, endovenous laser ablation, radiofrequency ablation, VenaSeal, and ClariVein. These vein treatments are safe, effective, and typically covered by insurance if medically necessary.
FAQs About Insurance and Vein Treatments
Do All Insurance Companies Cover Varicose Vein Treatments?
Not all insurance companies in the USA offer blanket coverage for varicose vein treatments. However, most will cover treatments deemed medically necessary. The key is to have a thorough medical evaluation that documents your symptoms and confirms a venous insufficiency diagnosis.
Does Insurance cover Spider Vein Treatments?
Spider vein treatments are often considered cosmetic and may not be covered. However, if they are related to venous insufficiency, the treatment for their root cause is usually eligible for coverage. In such cases, sclerotherapy spider vein treatment may also be covered as a part of the overall vein treatment plan.
Navigating insurance coverage for varicose vein treatments can feel overwhelming, but you don’t have to do it alone. At Vein Treatment Clinic, we make vein treatments accessible and affordable. Whether you’re dealing with varicose veins, spider veins, or venous insufficiency, our dedicated team is here to support you every step of the way. Visit your nearest vein treatment clinic or contact us to schedule a consultation today.
FEATURED POSTS BY VEIN DOCTORS